Effective Project Management Strategies for Healthcare Professionals
In most industries, a project slip-up might hurt timelines or stretch budgets. But when human life is at stake, the gap between “important” and “critical” narro...
In most industries, a project slip-up might hurt timelines or stretch budgets. But when human life is at stake, the gap between “important” and “critical” narrows down to a fine line. Let’s talk about project management in healthcare.
💡 Getting started? Read project management basics first.
💊 Understanding Healthcare Project Management

Effective project management involves understanding unique industry challenges, mastering essential skills, and applying tailored strategies.
So, what is a “project,” then?
Traditionally, a project is any endeavor with a specific goal in mind. It’s a structured effort that requires careful planning, execution, and management.
In healthcare, projects could range from implementing new electronic health records systems to rolling out cutting-edge patient care protocols.
What makes healthcare projects different are unique objectives which include:
🔴 Enhancing outcomes of healthcare services.
🔴 Compliance with healthcare laws and standards.
🔴 Minimizing risks and ensuring safe care practices.
🔴 Increasing the availability of medical services.
🔴 Introducing new treatments and technologies to enhance patient care.
🔴 Optimizing resources for faster, more effective service.
🔴 Protecting sensitive health information against breaches.
🔴 Fostering teamwork among healthcare professionals.
🚧 Key Challenges in Healthcare Project Management
Healthcare projects face a lot of obstacles. Some like budget and scope creep are common across all types of projects. Other are unique to the domain:
Following laws and regulations: Healthcare changes fast, and so do its rules. Medical billing codes, health insurance policies, workforce regulations, building codes and standards — all these aspects create a challenging environment for PMs to navigate.
Resource allocation and staff management: Healthcare institutions often operate under tight budgets and timelines. That means making all available resources count is key. The fight for top talent is fierce, and keeping teams motivated under pressure? That's a skill in itself.
Maintaining patient privacy and data security: Healthcare projects often involve handling sensitive data. That means they need to stay compliant with a number of laws regulating the handling of patient data like HIPPA in the US or GDPR in the European Union.
Adapting to new tech: Medicine has always been one of those fields where technology evolves non-stop. We're talking everything from telemedicine to AI in diagnostics. But blending the cutting-edge with without sidelining what already works can be difficult.
Overcoming those obstacles takes a mix of tools, techniques, individual savvy, and team synergy. So, what skills and practices are we talking about?
💡 Essential Project Management Skills for Healthcare Professionals
In 2009, Atul Gawande's book "The Checklist Manifesto" showed that something as simple as a checklist can improve outcomes in high-stakes environments.
Gawande, a respected surgeon, dived deep into how checklists improve outcomes and cut down errors in operating rooms and ICUs.
It turns out, implementing a simple checklist can reduce surgical complications by up to 36% and decrease mortality rates by 47%.(1)
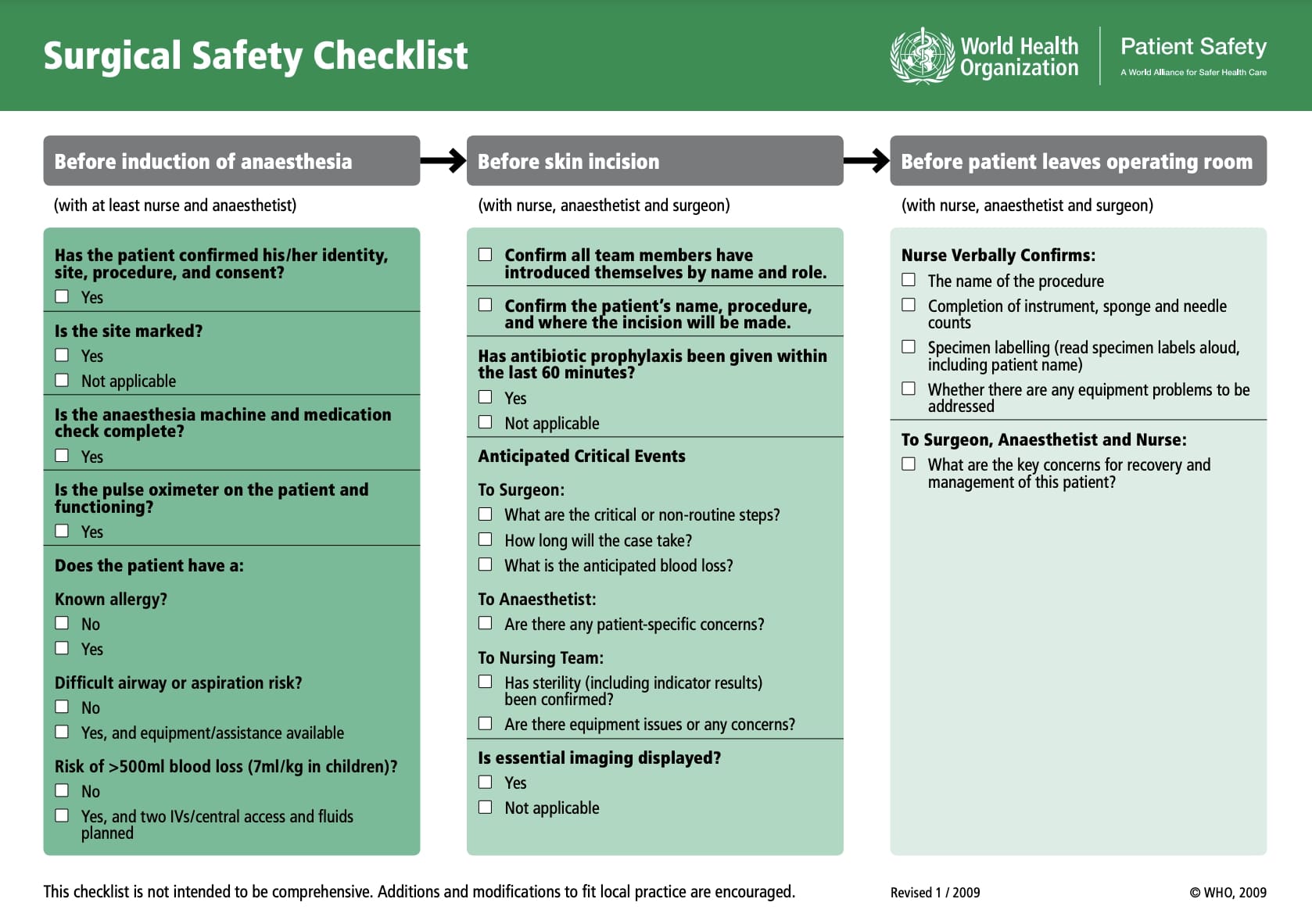
Surgical Safety Checklist. Source: WHO
Gawande’s take is a nod to broader, universal skills, some of which can be transferred to a healthcare setting. Take, for example, problem-solving.
The Cleveland Clinic Improvement Model, championed by Dr. Lisa Yerian, empowers caregivers to solve problems themselves, improving efficiency and patient care. It implements strategies and methodologies from the project management world to help staff to identify, discuss, and tackle issues directly.
The result?
Reduced pharmacy delivery times (from 10-14 days to under three days) and improved patient response times in a nursing unit by 23%.(2)
But it's not just problem-solving that makes the difference.
Communication skills bridge gaps between departments, leadership rallies medical staff through emergencies, and time management helps coordinate the life of a hospital facility. The skill transfer is more common than it may seem.
🛠️ Implementing Project Management in Healthcare
1. Building a Project Management Toolbox
Let’s say you're launching a telehealth platform.
The conventional approach would involve a chaotic blend of emails, spreadsheets, and whiteboards smothered with deadlines. The results? Project creep, budget overruns, and deadlines slipping through the cracks.
A centralized platform combining collaboration, communication, and planning will bring all that into focus. A consolidated view of tasks, milestones, and communications gives you a one-stop solution for:
Staff management
Compliance Tracking
Resource Allocation
Sharing documentation
Event planning
Internal communication
R&D coordination
All in one place, accessible 24/7 from any device, ensuring seamless integration and a unified approach to managing every aspect of your project.
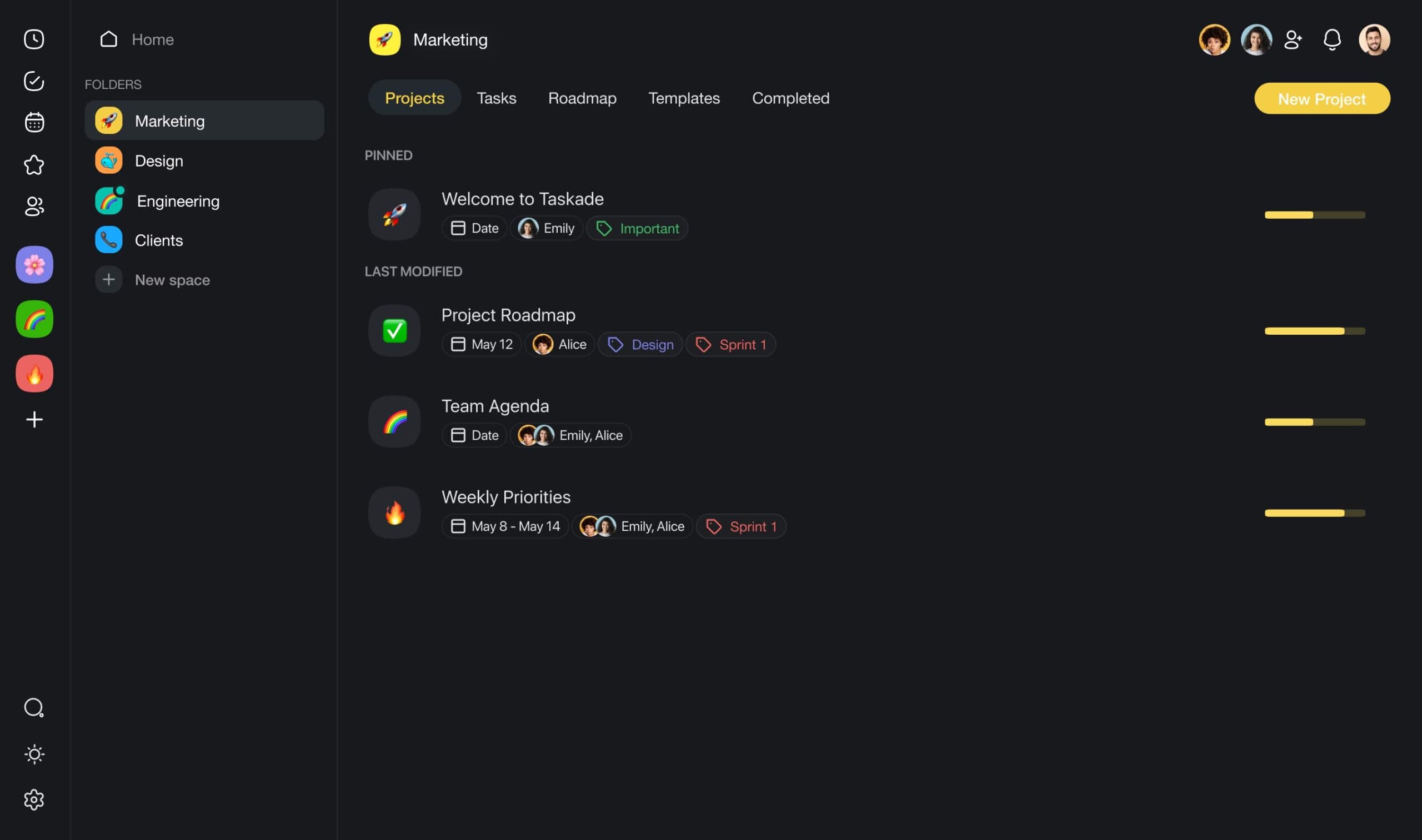
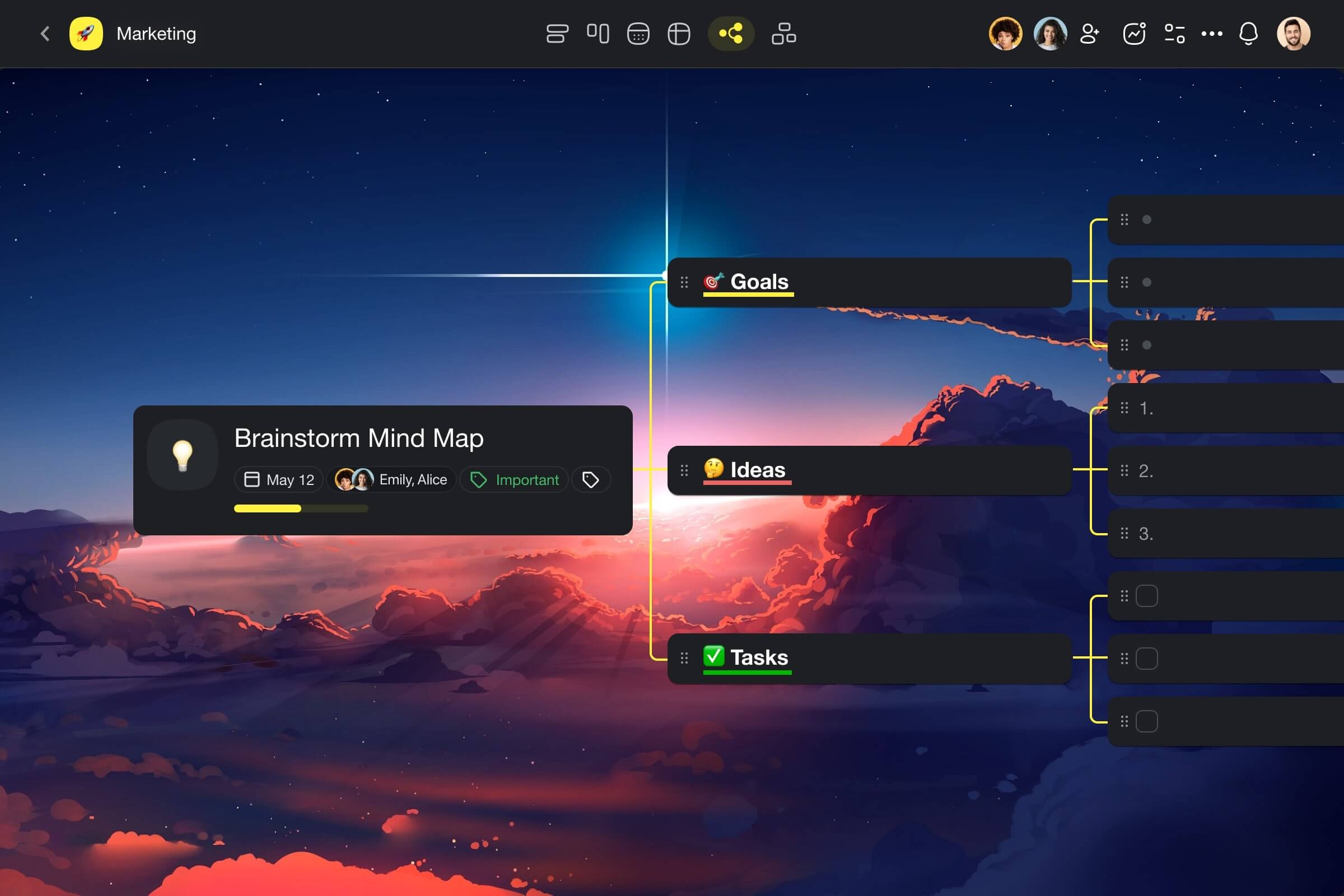
And speaking of tools... let us introduce Taskade. 🐑
Taskade is a holistic, AI-powered project management platform designed to streamline project workflows. It offers a unified space for managing tasks, tracking progress, and facilitating team communication.
With a laser focus on simplicity and integration, Taskade supports real-time collaboration, making it easier for teams to stay aligned and productive.
Want to learn more?
Sign up to transform your projects with Taskade AI
And now, let's get back to our topic.
2. Planning and Prioritization
With a project management toolbox in place, the next step is to lay out a detailed project plan. This step involves breaking down the project into manageable tasks, assigning responsibilities, and setting clear deadlines.
“How will the project enhance organization and patient care?”
“Which medical staff roles are pivotal in the early phases”
“How do we prioritize compliance with healthcare regulations”
There are project management techniques that will make the process faster:
Eisenhower Matrix: This method helps identify which tasks need immediate attention (urgent and important), which are important but not urgent (planning and development), which are urgent but not important (delegation), and which are neither urgent nor important (eliminate).
Pareto Analysis (80/20 Rule): According to the Pareto Principle, 80% of effects come from 20% of causes. For example, in healthcare project management, that can mean focusing on the 20% of tasks that will have the biggest impact on patient care and operational goals.
Priority Matrix: This technique sorts tasks into four sections to help decide what to focus on first. It identifies tasks that have a big impact but don't take much effort. This helps you see clearly what to prioritize, making it easier to manage your time and get things done efficiently.
Kano Model: Traditionally used in product development, the Kano Model can help prioritize features based on patient or stakeholder satisfaction. It groups features into must-be, one-dimensional, and delighters.
Of course, this is just the first step. We still have to pick the right project management methodology, but we'll get back to this in a moment.
3. Clearing Communication Hurdles
Data doesn’t lie — effective communication is the heartbeat of successful project management. According to the Project Management Institute (PMI), 29% of project failures are caused by poor communication.
When you're dealing with a multidisciplinary project team, clear, concise, and continuous communication is a must.
But it's easier said than done.
Let’s unpack some of the obstacles:
Silos between departments: Departments and specialized units often work in their own bubbles, causing information to slip through the cracks.
Language barriers: Medical staff use their own terms, while project managers have their own lingo. This affects how well people work together.
Resistance to change: Healthcare professionals may view new projects, especially those requiring changes to routines, with resistance.
Overreliance on email: While convenient, email can lead to information overload, with important messages getting lost in crowded inboxes.
Lack of real-time communication tools: Without tools that let people talk and make decisions quickly, projects can't move forward smoothly.
Addressing these challenges requires a proactive approach. Breaking down silos with cross-departmental meetings, simplifying language, and introducing change management techniques are all good starting points to consider.
🎛️ What Role Does Technology Play in Enhancing Project Management in Healthcare?
We’ve covered the role of project management platforms, which partly answers our question. But let’s take it a step further.
Since ChatGPT's debut in late 2022, generative AI has garnered significant attention. OpenAI's GPT-3 and GPT-4 have found their way into many industries, from customer service and logistics to education and finance.
There’s much talk of AI aiding in diagnosis or even robotic surgeons replacing doctors. But AI powers healthcare projects in a more subtle way.
For example, overstaffing generates costs, while understaffing might compromise patient outcomes. AI project management bots can optimize staffing by analyzing past shift patterns and predicting busy times.
Taskade's AI Agents are designed to streamline work and
automate repetitive parts of project workflows.
Next up: staff onboarding and training.
AI L&D platforms can offer a personalized experience based on roles and skills. A nurse might receive updates on patient care protocols, while a radiologist gets insights into new imaging techniques, all with instant feedback & support.
And that barely scratches the surface.
New tools like project management generators can revolutionize all kinds of healthcare projects, from clinical trials and improving organization at healthcare companies to supply chain optimization and public health initiatives.
💡 Want to learn more? Read AI predictive project management next.
🔄 Utilizing Project Management Methodologies in Healthcare
Whether it’s developing a new medical device, implementing an IT system, or improving patient care processes, each complex project has its unique challenges. And that means each requires a slightly different, tailored approach.
The project management world gives us many options.
Agile leverages flexibility, which makes it perfect for projects with shifting requirements. That can include developing EHR systems or patient portal apps. Its iterative nature allows for adaptation and continuous refinement.
Transitioning from Agile's flexibility, there's the more rigid Waterfall.
Waterfall offers a sequential, phase-based structure. It's ideal for projects with clear, more predictable stages and fixed requirements like building a healthcare facility or standardizing medical procedures across an organization.
If, however, you're looking for a steady optimization, there's Lean Six Sigma.
Lean Six Sigma is a methodology that focuses on improving processes by systematically eliminating defects and reducing variation. It combines principles from Lean manufacturing, which emphasizes efficiency and waste reduction.
Here’s how the three compare:
| Agile | Waterfall | Lean Six Sigma | |
|---|---|---|---|
| Philosophy | Emphasizes adaptability and flexibility to change. It's iterative and incremental. | Focuses on sequential and linear phases with no overlap. Each phase must be completed before the next begins. | Focuses on eliminating waste and defects to improve quality and efficiency. It combines Lean's waste elimination with Six Sigma's focus on quality control. |
| Process | Divided into sprints or iterations, allowing for regular reassessment and adjustments. | Divided into distinct phases: Requirements, Design, Implementation, Testing, Deployment, and Maintenance. No phase overlap. | Divided into five phases: Define, Measure, Analyze, Improve, and Control (DMAIC). This process focuses on understanding and reducing variation in processes. |
| Flexibility | High flexibility. Changes can be made late in the development process. | Low flexibility. Changes are difficult and costly once the project has advanced beyond the initial stages. | Moderate flexibility. Changes are encouraged early in the DMAIC process but become less feasible in later stages. |
| Feedback Loop | Continuous feedback through regular sprint reviews and retrospectives. | Feedback is usually gathered after project completion or at the end of each phase. | Continuous feedback during the Measure and Analyze phases to identify root causes of defects. |
| Project Duration | Can be more flexible with project duration due to iterative nature. | Typically has a fixed project duration determined at the start. | Duration can vary based on the complexity of the process being improved and the extent of the required changes. |
No one methodology fits all types of projects. That’s why healthcare projects might also use hybrid approaches, which could mean organizing a project with Waterfall but using Agile sprints to complete phases.
💡 Visit Agile vs. Waterfall for a detailed comparison.
Conclusion
Healthcare projects are about making every decision count, because at the end of the day, it's people's lives that are at stake. This comes with unique challenges, but it also leads to remarkable outcomes when done right.
We hope that the tips from this article will help you navigate the complexities of healthcare project management and bring your projects closer to success.
🔗 Resources
Sign up to transform your projects with Taskade AI